Osteomyelitis
Osteomyelitis is a serious and potentially debilitating infection of the bone. It occurs when bacteria or fungi invade the bone, leading to inflammation and destruction of bone tissue. This article aims to provide a comprehensive overview of osteomyelitis, including its causes, risk factors, common symptoms, and the importance of early diagnosis and treatment.
Understanding Osteomyelitis:
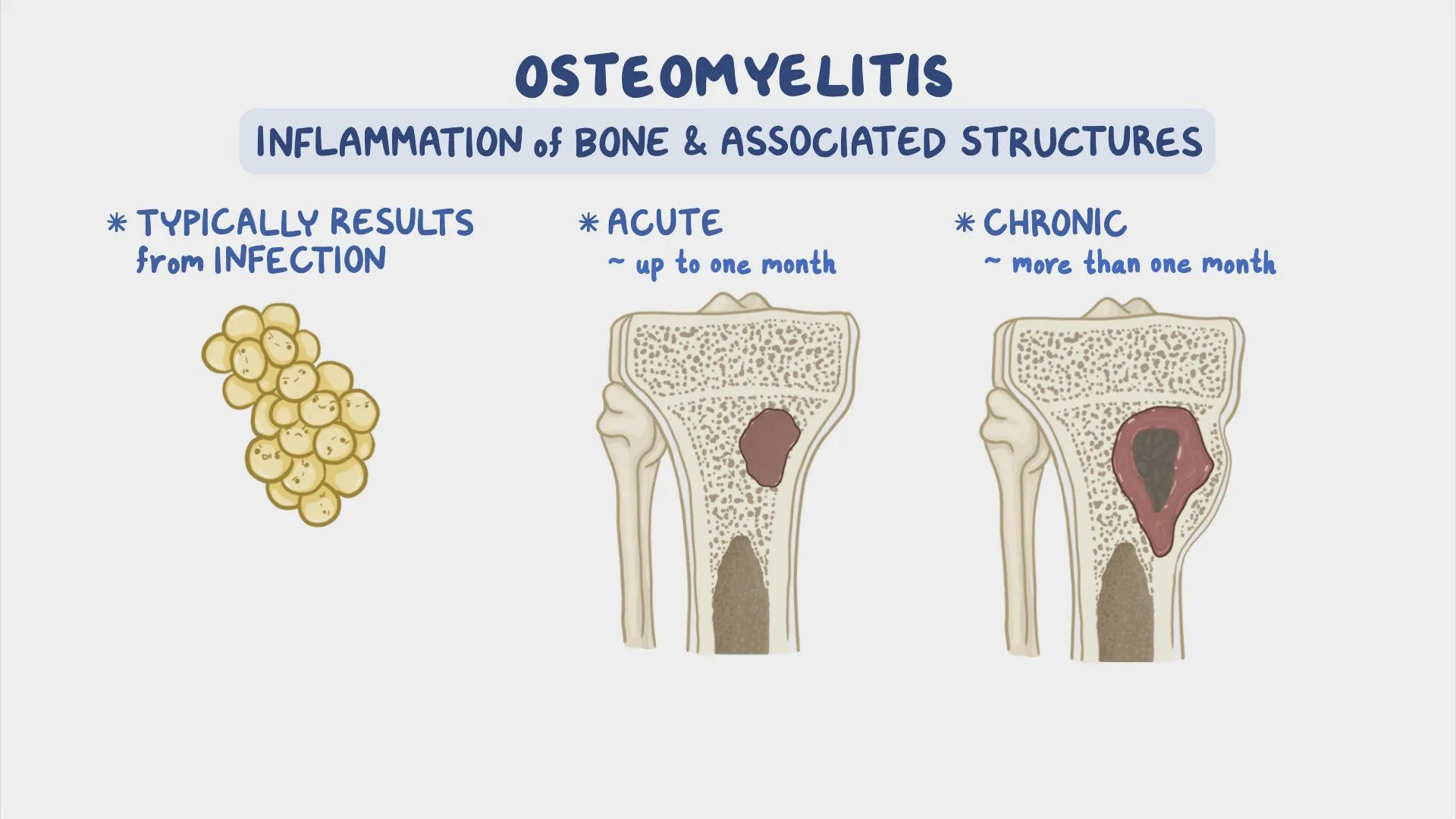
Osteomyelitis is an infection that can affect any bone in the body. It typically occurs when bacteria or fungi enter the bone through an open wound, surgical procedure, or bloodstream. Once inside the bone, the infectious agents multiply, leading to inflammation, bone destruction, and potential abscess formation. Osteomyelitis can be acute, developing rapidly and causing severe symptoms, or chronic, with a slower onset and milder symptoms.
Common Causes and Risk Factors:
a. Open Wounds and Trauma: Osteomyelitis can develop as a result of an open fracture, deep puncture wound, or surgical procedure involving bones.
b. Bloodstream Infections: Bacteria or fungi can travel through the bloodstream and reach the bone, particularly in individuals with weakened immune systems.
c. Pre-existing Infections: Infections in nearby tissues, such as a skin or soft tissue infection, can spread to the underlying bone.
d. Medical Conditions: Conditions such as diabetes, peripheral artery disease, and autoimmune disorders can increase the risk of developing osteomyelitis. e. Intravenous Drug Use: Sharing contaminated needles or injecting drugs directly into the bloodstream increases the risk of osteomyelitis.
Recognizing the Symptoms:
The symptoms of osteomyelitis can vary depending on the type (acute or chronic) and location of the infection. Common signs and symptoms include:
a. Localized Pain: Persistent and deep-seated pain in the affected bone, which may worsen with movement or pressure.
b. Swelling and Redness: The affected area may become swollen, warm to the touch, and exhibit redness or tenderness.
c. Limited Range of Motion: If the infection affects a joint, there may be a restriction in movement and stiffness.
d. Fever and Chills: In acute cases, individuals may experience a high fever, accompanied by chills and sweating.
e. Fatigue and Malaise: Systemic symptoms such as fatigue, general discomfort, and a feeling of unwellness may be present.
f. Wound Drainage: If the infection stems from an open wound, there may be pus or fluid draining from the affected area.
Importance of Early Diagnosis:
Early diagnosis of osteomyelitis is crucial to prevent complications and minimize the damage to bone tissue. Delayed or untreated osteomyelitis can lead to the following complications:
a. Bone Necrosis: The infection can cause bone tissue to die, resulting in areas of dead or non-functional bone.
b. Formation of Abscesses: Pockets of pus may form within the bone or surrounding soft tissues, requiring surgical drainage.
c. Spread of Infection: If left untreated, the infection can spread to nearby bones, joints, or even into the bloodstream, leading to a life-threatening condition called septicemia.
Diagnostic Methods:
To diagnose osteomyelitis, healthcare professionals employ several techniques, including:
a. Medical History and Physical Examination: The doctor will review the individual’s medical history, assess the symptoms, and perform a thorough physical examination.
b. Blood Tests: Blood samples are taken to identify the presence of infection by analyzing markers such as elevated white blood cell count and inflammatory markers.
c. Imaging Studies: X-rays, CT scans, or MRI scans can provide detailed images of the affected